While coronavirus (COVID-19), a disease caused by a novel virus, SARS-CoV-2, is best known for causing acute respiratory distress, some patients inflicted with the virus are developing serious cardiovascular issues. The coronavirus enters the body’s cells through the angiotensin converting enzyme 2 (ACE2) receptor that helps regulate blood pressure and the vascular permeability, or the capacity of the blood vessel wall to allow for the flow of small molecules such as water and nutrients, including the blood vessels prevalent in the lungs and heart. COVID-19 may also cause endotheliitis, an inflammation of the tissue lining the blood vessels as well as the heart, causing a massive inflammatory response leading to the formation of blood clots.1 This may explain why people with COVID-19 experience a sudden deterioration of their respiratory function and shortness of breath.
Causes of cardiac injury in COVID-19 patients
SARS-CoV-2 infection may also increase permeability of the blood vessels through the ACE2 receptor leading to an escalation in swelling and inflammation. In its most severe stage, a massive inflammation typically leads to extensive pulmonary damage with a subsequent lack of oxygen and finally multiorgan failure.2 This very strong response by the immune system has also been called the cytokine storm and it may initiate more damage than the virus itself, causing some of the young COVID-19 patients to be severely affected.
A high incidence of acute myocardial injury--likely around 20 percent--is associated with poor prognosis and therefore a potential target for aggressive treatment.3 According to early reports, up to 50 percent of COVID-19 patients with acute myocardial injury may die.3 The primary cardiac injuries occurring in COVID-19 patients are acute myocarditis, an inflammation of heart muscle, or acute myocardial infarction, also known as a heart attack.
Using Cardiac MR (CMR) for COVID-19
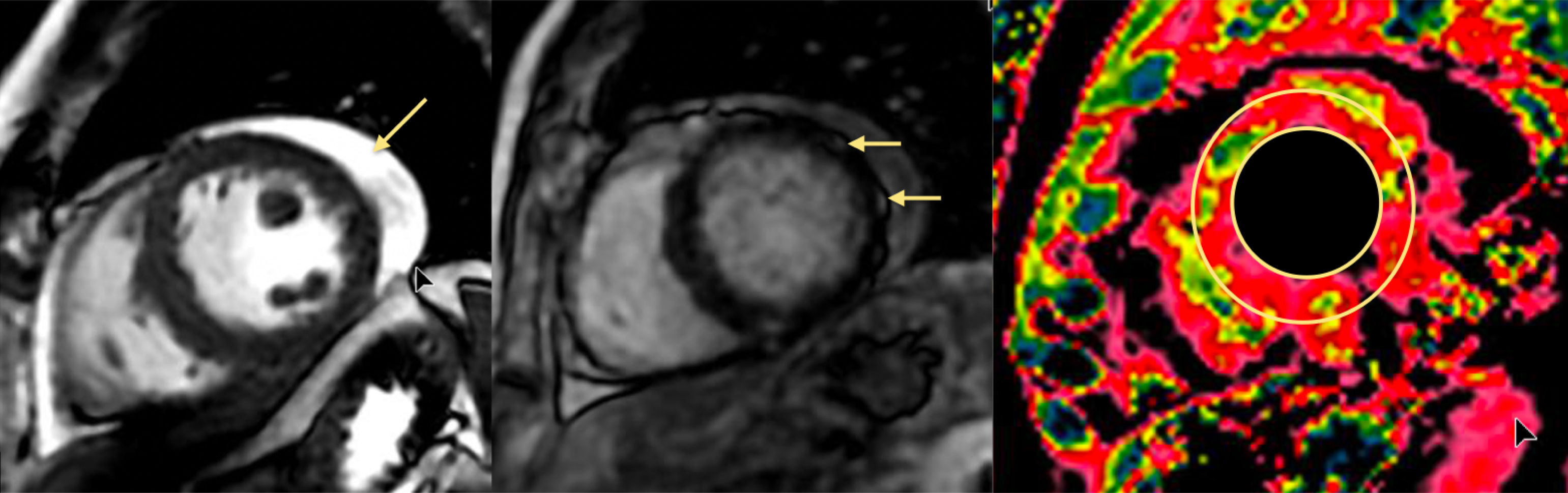
A recently published consensus paper from three leading medical associations recommends additional noninvasive evaluation in patients with an unclear or unequivocal diagnosis. Potential causes for myocardial injury can be ST-elevation myocardial infarction (STEMI), viral invasion itself, the inflammatory response of an overly active immune system or a mismatch systemic of oxygen supply and demand.4 Among various non-invasive diagnostic procedures, cardiac MR (CMR) has a unique potential for visualizing the heart’s anatomy, function and viability; for certain conditions it may provide the best images of the heart.5
Although CMR is one of several imaging techniques that can be utilized for COVID-19 patients with suspected acute myocardial injury, it is the best technique for improved soft tissue definition to look for tissue injury and to visualize tissue pathology. CMR can help identify ischemic versus non-ischemic injury6 and is considered the noninvasive gold standard for verifying or refuting a diagnosis of acute myocarditis using late gadolinium enhancement.
Impact of CMR on clinical decision making
COVID-19 patients with clinical suspicion of acute myocardial injury should be frequently (every 24 to 48 hours) checked for ST elevation in ECG, shortness of breath not otherwise explained, arrhythmia or atypical chest pain. Troponin, a sensitive serologic marker, should be measured in all patients with suspected acute myocardial injury. If troponin is elevated, a cardiac MR scan can help differentiate normal from acute non-ischemic injury. Furthermore, it can also help differentiate between numerous non-ischemic myocardial diseases. CMR has been shown to have a strong impact on clinical decision making, such as whether the patient goes to cardiac catheterization or receives aggressive heart failure treatment, and, therefore, also on patient outcomes.7 If the heart appears relatively normal on CMR then further diagnostic testing for other underlying causes, e.g., lung injury, is warranted. The Society for Cardiac Magnetic Resonance (SCMR) has published guidance for the use of CMR during the COVID-19 pandemic.8
One additional and important aspect regarding the use of MR in COVID-19 patients is that it can be used to examine other organs. In one scan, MR could double rule-out both pulmonary and cardiac involvement without the use of contrast, thereby avoiding additional patient transport through the hospital for a separate diagnostic imaging study and possibly save precious therapeutic decision-making time.
*New information regarding COVID-19 continues to emerge daily. This content was based on the sources available at the time of writing.
References
- Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417‐1418. doi:10.1016/S0140-6736(20)30937-5.
- Akhmerov A, Marbán E. COVID-19 and the Heart. Circ Res. 2020;126(10):1443‐1455. doi:10.1161/CIRCRESAHA.120.317055.
- Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) [published online March 27, 2020].JAMA Cardiol. 2020. doi: 10.1001/jamacardio.2020.1017. https://jamanetwork.com/journals/jamacardiology/fullarticle/2763845.
- Mahmud E, Dauerman HL Frederick GP, et al. Management of Acute Myocardial Infarction During the COVID-19 Pandemic. J Am Coll Cardiol. 2020 Apr 30. Epublished DOI:10.1016/j.jacc.2020.04.039.
- Radiologyinfo.org. Magnetic Resonance Imaging (MRI) – Cardiac (Heart). Available at: https://www.radiologyinfo.org/en/info.cfm?pg=cardiacmr.
- Sanz J. Evolving diagnostic and prognostic imaging of the various cardiomyopathies. Ann N Y Acad Sci. 2012;1254:123‐130. doi:10.1111/j.1749-6632.2012.06490.x
- Moschetti K, Favre D, Pinget C, Pilz G, Petersen SE, Wagner A, Wasserfallen JB, Schwitter JJ. Comparative cost-effectiveness analyses of cardiovascular magnetic resonance and coronary angiography combined with fractional flow reserve for the diagnosis of coronary artery disease. J Cardiovasc Magn Reson 2014;16:13.
- Han Y, Chen T, Bryant J, et al. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. J Cardiovasc Magn Reson. 2020;22(1):26. Published 2020 Apr 27. doi:10.1186/s12968-020-00628-w.